Myopia Management Program
Myopia Management Program
Myopia worldwide is reaching epidemic levels and with this explosion comes more eye disease. What can we do to stop it!?
At Precision Family Eye Care, we understand the importance of preserving sight and maximizing visual function. One of the most common conditions we see in daily practice is myopia (trouble seeing far away). For far too long, myopia progression in children has been considered a largely benign finding requiring no more than simply “getting new glasses” or “updating the contact lenses.” In reality, progressive myopia in children can have profound impacts on both the quality of life as well as ballooning the life-time risks of serious sight threatening ocular disease. Fortunately, there are several extremely successful ways of controlling the progressive nature of of myopia. There is no one size fits all approach and often times we will employ multiple options.

The Myopia Epidemic
It's Bigger than you Think!
Myopia rates in the United States were 24% in the early 1970s, however, by the early 2000s, that number was 44%! (2). And the problem isn’t isolated to the United States. East Asian countries are the most extensively effected; with dizzying myopia rates of as high as 80-90% of college educated adults. The world as a whole is simply getting more and more myopic. In 2010, 28% of the globe was myopic and viewing the current trends of the myopia surge, it is estimated that over 50% of all humans will suffer from myopia by 2050 (1).
What is Myopia?
When does it usually develop?
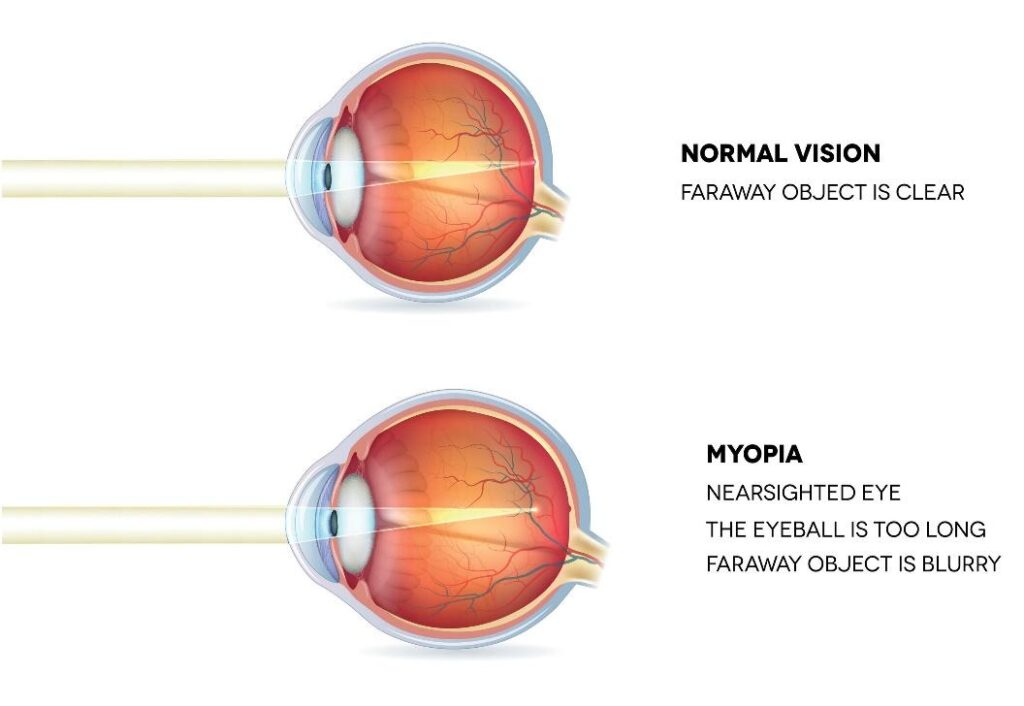
Simply put, myopia or near-sightedness is caused by a longer eyeball than nature intended. There are two main types of myopia, spontaneous onset myopia and pathological myopia. Pathological myopia features extreme progression of myopia and eye length growth that often continues throughout life. Thankful pathological myopia is relatively uncommon affecting 0.9-3.3% of the population (3). Far more common is spontaneous onset myopia, also known as school age myopia. Ages 6 through 16 is considered the “golden age” for spontaneous myopia progression and most nearsightedness that develops throughout our lifetime will occur during this period. As a child is becoming more myopic, the globe grows, getting longer front to back. We refer to this type of growth as axial elongation. As the eye lengthens, the light no longer focuses on the retina and causes blurry, decreased vision in the distance. As a result, higher powered glasses/contacts are prescribed to the account for this change.
But WHY does Myopia Develop?
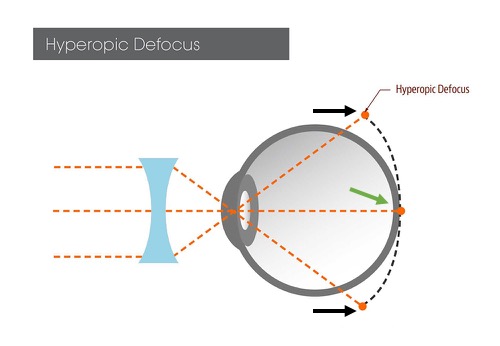
Understanding Hyperopic Defocus
The underlying mechanism that causes myopia is called Peripheral Hyperopic Defocus. As noted above, glasses and traditional contact lenses focus the light back onto the center of the retina where central (20/20) vision is located allowing clear distance vision (Green arrow). However, way glasses/contact refract light cause the light hitting the peripheral parts retinal to focus behind the retina (white arrows left), hence Peripheral Defocus. Research suggests that it’s the outside areas of the retina that control eye growth. Since the peripheral retina is receiving a blurry, out of focus image, the eye elongates. However, when the eye elongates the glasses are no longer presenting a clear image to central part of the retina and a new, stronger prescription is needed. This rinse-and-repeat cycle often continues throughout childhood resulting in more and more myopia
What are the Risk Factors for Developing Myopia?
Current Research for the Nerds Like Me!
While we know the physical reason that myopia develops. The risk factors that predispose the eye to grow in the first place is quite a bit murkier. There are a variety of scientifically proven risk factors. Some of these risk factors are modifiable while others are not. Known risk factors include:
The earlier a child begins to develop myopia, the faster and more severe the progression often occurs (4,5). For example, children who begin developing myopia before age 13 are orders of magnitude more likely to have high myopia later in life compared to a college student getting their first pair of glasses.
As with many medical conditions, genetics and ethnicity are also associated with myopia development.
Myopia in the Parents (7)
- If Neither parent is myopic, the myopia risk for their children is 7%
- If One parent is myopic, the myopia risk for their children is 17%
- If Both parents are myopic, the myopia risk for their children is 40%
Myopia Percentage by Ethnicity of 6 year olds in the United States (22,23) .
- Non-Hispanic white - 1.2%
- Hispanic white - 3.7%
- Asian - 3.98%
- African American - 6.6%
This is likely a proxy measurement for a variety of things but the literature is clear that these are risk factors (8,9,10)
- Higher levels of education
- Better housing
- Higher income
- Occupations associated with extensive near work
From looking at the literature, it is clear that near work DOES increase the risk of myopia development AND progression.
This association seems stronger with electronic devices (tablets, cell phones, video games devices), when holding things closer than appropriate to read, and with extended periods of near work without taking breaks.
Relevant Studies
- In one study (11), children who read more than two books per week were 3x more likely to develop myopia. This same study found that reading more than 2 hours a day was not associated with myopia progression.
- Another study (12) found that more than 3 hours per day spent on a digital device, on specifically a digital device caused a 2-to-3-fold increase in the development of myopia, in one study with as little as 30-60 minutes of use per day (13).
- The Sydney Adolescent Vascular and Eye Study (SAVES) (14) found that children who became myopic performed two more hours of near work per week than patients who did not become myopic. Although this effect was not as clear or strong for older children.
- There seems to be an association with the duration of continuous near work rather than cumulative duration of near work. Additionally, shorter reading distances have been correlated with faster myopic progression (15).
It has long been suggested that outdoor play reduces the risk of myopia progression in children, research agrees!
“Outdoor activity reduces the prevalence of myopia in children”(16) Conclusions
- 12-year-olds with higher levels of outdoor activity had lower myopia prevalence
- Children with high levels of near work AND low levels of outdoor activity had the most myopia.
- Conversely, children with low levels of near work AND high levels of outdoor activity had the least amount of myopia.
- Regardless of near tasks, children with higher levels of outdoor activity had the lowest risks of myopia
- In the younger children, ages 6 and younger, outdoor time was NOT associated with myopia progression16.
A study of 7 – 12 year-old children found that children who had two additional hours of outdoor activity a week were half as likely to develop myopia (17).
A meta-analysis of seven studies looking at outdoor time and myopia development, concluded that the risk of development and progression of myopia decreased by 2% per additional hour of outdoor time a week (18).
Possible mechanisms? - While this association is clear, the cause is less understood.
- Increased sunlight from outdoor time leads to dopamine release, dopamine release is hypothesized to thicken the globe of the eye which decreases axial elongation reducing myopia prevalence (16,19).
- Visual targets outdoors are typically more diverse and farther away than indoors where objects are closer and cause more hyperopic defocus (20)
- Vitamin D (vitamin made by the skin during sun exposure): While this is likely more correlation than causation, myopic individuals have lower levels of Vitamin D vision normal individuals.
Why does Preventing Myopia Progression Matter?
In short... its ALL about eye disease.
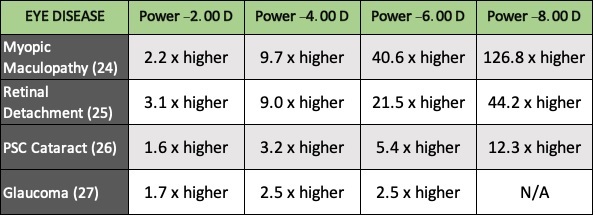
As seen in the chart below, small amounts of myopia don’t dramatically increase the relative risks of developing eye disease. High myopia (defined as > -5.00 D of myopia), however, balloons the risk of several myopia related eye disease to uncomfortable levels. With the rates of myopia and high myopia on the rise worldwide, the goal of the myopia control program in children is to reduce the myopia developed during the formative years thus reducing the risk of serious ocular disease complications later in life.
Treatment Choices for Myopia Control
We have Options!
Typically, soft bifocal contact lenses have been used to help contact lens wearers to see up close when near vision begins to fade during the 40’s and 50’s. These lenses are used in myopia control because they decrease hyperopic defocus which is known to accelerate eye growth and myopia (24).
There are several types of Bifocal or Multifocal Contact lenses available for us to try. Even though most bifocal lenses are not FDA approved for myopia control specifically, there are many studies that laud the effectiveness of this treatment approach (25, 26, 27). In 2020, the first Dual Focus contact lens called 1Day MiSight was FDA approved for the purpose of myopia management in the United States.
Soft Bifocal Contact Lenses reduce the risk of Myopia Progression by 45-55%
Orthokeratology (ortho-k) also known as Corneal Reshaping Therapy (CRT) is a non-surgical method of reshaping the front of the cornea to correct for myopia refractive errors. This is accomplished by having the patient where a hard contact lens overnight while asleep. Think of it as a retainer, but for the eyes. During sleep the hard lens gently flattens the central cornea shape. When the lens is removed in the morning, no glasses or contact lenses are needed during the day. The lens is then reused at night to maintain the slightly flattened corneal curvature.
Because of the way an Orthokeratology lens molds the surface of the eye, the resultant corneal shape causes a decrease in hyperopic defocus landing on the retina (30). Therefore, in addition to not having to wear glasses during the day, Orthokeratology has also been shown to be highly effective in the prevention of myopia progression (28, 29).
Orthokeratology reduces the risk of Myopia Progression by 41-51%
Atropine is one medication in a family of medicines used in eyecare to dilate the pupil and temporarily paralyze the focusing system to better visualize the internal parts of eye. The theory of how these medications slow the progression of myopia is unclear and there are several hypotheses from causing dopamine release to causing thickening of the wall of the eyeball (32-37). Regardless of how it curtails myopia progression, it is exceedingly effective. Standard 1% atropine dosing locks down the development of myopia by 80-90%. Unfortunately, high concentration atropine causes significant visual side effects and significant myopia rebound when atropine therapy is stopped (38,39). Diluted solutions of atropine, while not as effective, still show a strong ability stop myopia progression with little to know visual side effects and minimal rebound in myopia progression after discontinuing the eye drop (40,41).
Low dose atropine (0.05 to 0.01%) reduces the risk of Myopia Progression by 40-50%
References
(1) World Health Organization. The High Impact of Myopia and High Myopia. WHO; 2017. Accessed Nov. 14, 2019.
(2) Bressler NM. Reducing the Progression of Myopia. 2020;324(6):558–559. doi:10.1001/jama.2020.10953
(3) Y. Wong, A. Ferreira, R. Hughes and et al, "Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review.," Am J Ophthalmol, vol. 157, no. 1, pp. 9-25, 2014.
(4)zadnik, S. A. Cotter, L. A. Jones-Jordan and et al, "Prediction of Juvenile-Onset Myopia.," JAMA Ophthalmol, vol. 133, no. 6, pp. 683-9, 2015.
(5) Y. Chua, C. Sabanayagam, Y. B. Cheung and et al, "Chua SY, Sabanayagam C, Cheung YB, Chia A, Valenzuela RK, Tan D, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children.," Ophthalmic Physiol Opt, vol. 36, no. 4, pp. 388-94, 2016.
(6) O. Mutti, G. L. Mitchell, M. L. Moeschberger and et al, "Parental myopia, near work, school achievement, and children's refractive error," Invest Ophthalmol Vis Sci, vol. 43, no. 12, pp. 3633- 3640, 2002.
(7) M. Ip, S. C. Huynh, D. Robaei and et al, "Ethnic differences in the impact of parental myopia: findings from a population-based study of 12-year-old Australian children," Invest Ophthalmol Vis Sci, vol. 48, no. 6, pp. 2520-2528, 2007.
(8) M. M. I. Xiang F, "The impact of parental myopia on myopia in Chinese children: populationbased evidence," Optom Vis Sci, vol. 89, no. 10, pp. 1487-1496, 2012.
(9) P. J. G. S. S. Wong TY, "Refractive errors, axial ocular dimensions, and age-related cataracts: the Tanjong Pagar survey," Invest Ophthalmol Vis Sci, vol. 44, no. 4, p. 1479–1485, 2003.
(10) J. H. S. L. S. Lim HT, "Prevalence and associated sociodemographic factors of myopia in Korean children: the 2005 third Korea National Health and Nutrition Examination Survey (KNHANES III)," Jpn J Ophthalmol, vol. 56, no. 1, pp. 76-81, 2012.
(11) M. Saw, W. H. Chua, C. Y. Hong and et al, "Nearwork in early-onset myopia," Invest Ophthalmol Vis Sci, vol. 43, no. 2, pp. 332-339, 2002.
(12) Lanca and S. M. Saw, "The association between digital screen time and myopia: A systematic review.," Ophthalmic Physiol Opt, vol. 40, pp. 216-229, 2020.
(13) Saxena, P. Vashist, R. Tandon and et al, "Incidence and progression of myopia and associated factors in urban school children in Delhi: The North India Myopia Study (NIM Study).," PLoS One, vol. 12, no. 12, p. e0189774, 2017.
(14) N. French, I. G. Morgan, G. Burlutsky and et al, "Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren.," Ophthalmology, vol. 120, no. 7, p. 1482–1491, 2013.
(15) C. Huang, Y. C. Hsiao, C. Y. Tsai and et al, "Protective behaviours of near work and time outdoors in myopia prevalence and progression in myopic children: a 2-year prospective population study.," Br J Ophthalmol, vol. 104, no. 7, 2019.
(16) A. Rose, I. G. Morgan, J. Ip and et al, "Outdoor activity reduces the prevalence of myopia in children," Ophthalmology, vol. 115, no. 8, pp. 1279-1285, 2008.
(17)C. Wu, C. L. Tsai, H. L. Wu and et al, "Outdoor Activity during Class Recess Reduces Myopia Onset and Progression in School Children," Ophthalmology, vol. 120, no. 5, pp. 1080-1085, 2013.
(18) C. Sherwin, M. H. Reacheer, R. H. Keogh and et al, "The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis," Ophthalmology, vol. 119, no. 10, pp. 2141-2151, 2012.
(19) L. Megaw, M. G. Boelen, I. G. Morgan and et al, "Diurnal patterns of dopamine release in chicken retina," Neurochem Int, vol. 48, no. 1, pp. 17-23, 2006.
(20) A. Choi, K. Han, Y.-M. Park and T. Y. La, "Low Serum 25-Hydroxyvitamin D Is Associated With Myopia in Korean Adolescents Serum Vitamin D in Myopia.," Investigative ophthalmology & visual science, vol. 55, no. 4, pp. 2041-7, 2014.
(21) Cuellar-Partida, K. M. Williams, S. Yazar and et al, "Genetically low vitamin D concentrations and myopic refractive error: a Mendelian randomization study.," International journal of epidemiology, vol. 46, no. 6, pp. 1882-90, 2017.
(22) Wen, K. Tarczy-Hornoch, R. McKean-Cowdin and et al, "Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: multi-ethnic pediatric eye disease study.," Ophthalmology, vol. 120, no. 10, pp. 2109-16, 2013
(23) Multi-Ethnic Pediatric Eye Disease Study Group, "Prevalence of myopia and hyperopia in 6- to 72- month-old african american and Hispanic children: the multi-ethnic pediatric eye disease study.," Ophthalmology, vol. 117, no. 1, pp. 140-147, 2010.
(24) A. Ticak and J. J. Walline, "Peripheral optics with bifocal soft and corneal reshaping contact lenses," Optom Vis Sci, vol. 90, no. 1, pp. 3-8, 2013.
(25) J. J. Walline, K. L. Greiner, M. E. McVey and et al, "Multifocal contact lens myopia control," Optom Vis Sci, vol. 90, no. 11, pp. 1207-1214, 2013.
(26) T. A. Aller, M. Liu and G. F. Wildsoet, "Myopia Control with Bifocal Contact Lenses: A Randomized Clinical Trial," Optom Vis Sci, vol. 93, no. 4, pp. 344-352, 2016.
(27) P. Chamberlain, S. C. Peixoto-de-Matos, N. S. Logan and C. Ngo, "A 3-year Randomized Clinical Trial of MiSight Lenses for Myopia Control," Optom Vis Sci ., vol. 96, no. 8, pp. 556-567, 2019.
(28) D. Wen, J. Huang, H. Chen and et al, "Efficacy and Acceptability of Orthokeratology for Slowing Myopic Progression in Children: A Systematic Review and Meta-Analysis," Journal of Ophthalmology, 2015.
(29) C. Chen, S. W. Cheung and P. Cho, "Myopia control using toric orthokeratology (TO-SEE study).," Invest Ophthalmol Vis Sci, vol. 54, pp. 6510-17, 2013.
(30) T. Kakita, T. Hiraoka and T. Oshika, "Influence of overnight orthokeratology on axial elongation in childhood myopia," Invest Ophthalmol Vis Sci, vol. 52, no. 5, pp. 2170-2174, 2011.
(31) N. A. McBrien, W. K. Stell and B. Carr, "How does atropine exert its anti-myopia effects?," Ophthalmic and Physiological Optics, vol. 33, no. 3, pp. 373-378, 2013.
(32) H. N. Schwahn, H. Kaymak and F. Schaeffel, "Effects of atropine on refractive development, dopamine release, and slow retinal potentials in the chick.," Vis Neurosci, vol. 17, pp. 165-176, 2000.
(33) D. L. Nickla, X. Zhu and J. Wallman, "Effects of muscarinic agents on chick choroids in intact eyes and eyecups: evidence for a muscarinic mechanism in choroidal thinning.," Ophthalmic Physiol, vol. 33, pp. 245-256, 2013.
(34) K. Ayajiki, T. Tanaka, T. Okamura and N. Toda, "Evidence for nitroxidergic innervation in monkey ophthalmic arteries in vivo and in vitro," American Journal of Physiology-Heart and Circulatory Physiology, vol. 279, no. 4, pp. H206-12, 2000. 43 Vision Source
(35). N. Toda and M. Nakanishitoda, "Nitric oxide: ocular blood flow, glaucoma, and diabetic retinopathy,," Progress in Retinal and Eye Research, vol. 26, no. 3, pp. 205-238, 2007.
(36) G. J. Lind, S. J. Chew, D. Marzani and et al, "Muscarinic acetylcholine receptor antagonists inhibit chick scleral chondrocytes," Invest Ophthalmol Vis Sci, vol. 39, pp. 2217-2231, 1998.
(37) V. A. Barathi and R. W. Beuerman, "Molecular mechanisms of muscarinic receptors in mouse scleral fibroblasts: prior to and after induction of experimental myopia with atropine treatment.," Mol Vis, vol. 17, pp. 680-92, 2011
(38) W. H. Chua and et al, "Atropine for the treatment of childhood myopia. (ATOM1)," Ophthalmology, vol. 113, pp. 2285-2291, 2006.
(39) L. Tong, X. L. Huang, A. L. Koh and et al, "Atropine for the treatment of childhood myopia: effect on myopia progression after cessation of atropine," Ophthalmology, vol. 116, pp. 572-579, 2009.
(40) A. Chia, W. H. Chua, Y. B. Cheung and et al, "Atropine for the treatment of childhood Myopia: Safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2)," Ophthalmology, vol. 119, pp. 347-354, 2012.
(41) J. C. Yam, F. L. MMed, X. Zhang, S. M. Tang and et al, "Two-Year Clinical Trial of the LowConcentration Atropine for Myopia Progression (LAMP) Study: Phase 2 Report," Ophtalmology, vol. 127, no. 7, pp. 910-919 , 2020.
Is your child ready to become a member of our Myopia Control Program family?
We're ready to help get your child on the path to minimizing myopia and the ocular health consequences that may result. Schedule your appointment for evaluation today!
